A third patient was reported HIV-free this week after receiving a stem cell transplant. Here’s everything you need to know about the procedure.
A study published February 9 declared a third person free of HIV after receiving a specific type of bone marrow, or stem cell, transplant. The 53-year-old man, who researchers are calling the “Düsseldorf” patient, received the treatment in 2013 and has been monitored since.
Like the two others — known as the “Berlin” and “London” patients, respectively — the man was positive for Type 1 HIV (HIV-1) and received a specific type of stem cell transplant to help treat a cancer diagnosis.
Both the Düsseldorf and Berlin patients had leukemia, while the London patient had Hodgkin’s lymphoma.
What are stem cells?
“Stem cell” is an umbrella term that refers to cells that are constantly dividing and have the potential to form different cell types.
Most of the body’s cells are very specialized and can’t change type — they will be stuck as heart muscle cells, neurons or intestine wall cells for the rest of their “lives”.
In contrast, stem cells are more like teenagers about to graduate high school.
They have the potential to become pretty much anything — a lawyer, nurse, scientist, journalist, influencer or TikToker — and must adapt to new trends.
What are hematopoietic stem cells?
The three HIV-free patients all received an allogenic hematopoietic stem cell (HSC) transplant.
The terms “bone marrow” and “stem cell” are often used interchangeably when talking about this procedure, because there are HSCs in our bone marrow.
HSCs are a cell-producing machinery that can give rise to blood and immune system cells through a process called hematopoiesis, which comes from two Greek words that together mean “blood making”.
You might not realize it, but every day HSCs produce around 300 billion new cells in your bone marrow.
Different types of stem cells
But not all teenagers are equally flexible when it comes to figuring out what they want to become. Some may be really into art, while others may be passionate about science and incapable of drawing a tree.
Stem cells also have different types of potential. Some can generate many different cell types, while others only a few.
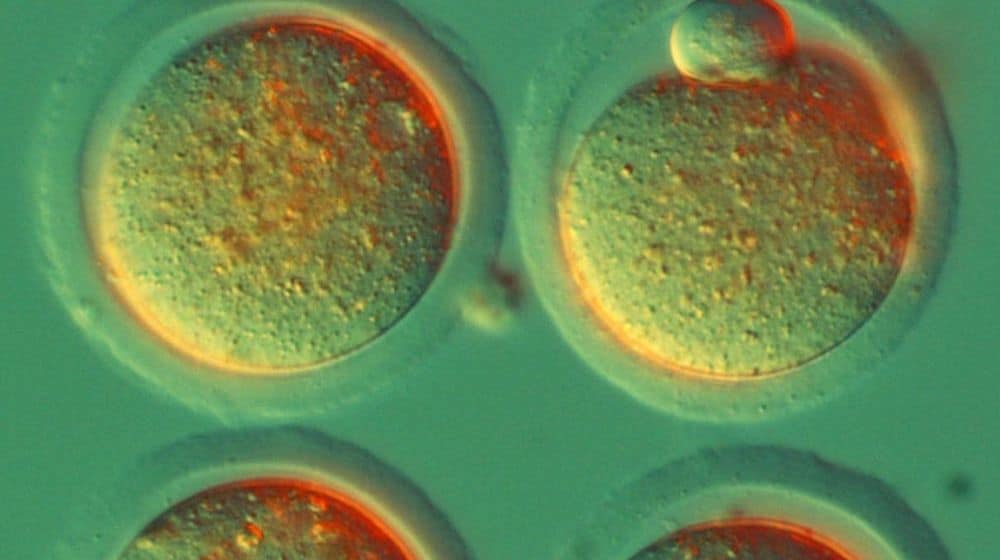
Pluripotent stem cells can generate all the different types of cells required for an embryo to develop. Multipotent stem cells, on the other hand, can only generate a few types of cells.
Adult humans have multipotent stem cells in parts of the body where the cells need constant replenishment, like the skin, bones and gonads.
Scientists received the Nobel Prize in 2012 after proving it’s possible to manipulate already-differentiated cells into becoming pluripotent again through a process called “cell reprogramming”.
Since then, stem cell therapy has become a very active field of research.
Hematopoietic stem cell transplant
There are several types of stem cell therapies, and despite being harsh and risky, the HSC transplant is the most popular.
The procedure attempts to fix unhealthy bone marrow by replacing it with healthy marrow from a donor. It treats conditions that are often life-threatening, like certain types of cancers or blood/immune disorders such as sickle cell disease.
Stem cell transplants are classified by the origin of the stem cells that are being transplanted. For example, if the cells come from the body of the person who is being treated, the procedure is called an autologous stem cell transplant. If they come from someone else, it’s considered allogenic.
Each of the three HIV-free patients received an allogenic HSC transplant.
A high-risk transplant
Before receiving an HSC transplant, a patient is required to undergo a harsh “conditioning” regimen, which can include chemotherapy and radiotherapy.
Both treatments can have serious side effects, like infections, organ failure and even death. They are conducted in order to destroy the patient’s unhealthy bone marrow and heavily suppress their immune system, which allows the transplant to properly integrate.
If the treatment is successful, the transplanted cells will trigger an immune reaction against any residual cancer cells, helping clear them in what’s called a graft-versus-tumor effect.
But things can go awry. In some cases, the donor’s transplanted immune cells may start to recognize the recipient’s body as foreign and attack it, leading to graft-versus-host disease.
Graft-versus-host disease can affect the skin, the intestines and the liver. In some cases, it can even be life-threatening.
Not a treatment for HIV
Due to its high risk, researchers from the three HIV-remission studies have repeatedly cautioned that HSC transplants should not be seen as a treatment for HIV, which can be well managed with anti-retroviral treatment.
Researchers across the world are still looking for a cure or vaccine for the virus.